Principal Investigators : Nicolas Cabé, Laurent Coulbault, Alice Laniepce, Anne-Lise Pitel
The axis of alcohol use disorder addresses 6 themes:
- Physical activity PI: Nicolas Cabé
- Biomarkers PI: Laurent Coulbault
- Sleep disorders PI: Alice Laniepce
- Cognitive and brain pathophysiology PI: Anne-Lise Pitel (collaboration Shailendra Segobin, Inserm U1077)
- Korsakoff’s syndrome PI: Anne-Lise Pitel (collaboration Shailendra Segobin, Inserm U1077)
- Alcohol and aging PI: Anne-Lise Pitel
Physical activity
Leader : Nicolas Cabé
Physical activity is a promising adjunctive treatment of severe alcohol use disorder (AUD). This is a low-cost, low-risk treatment that is not perceived as stigmatizing by patients. It could help improve both the physical and mental health of patients and reduce their sedentary behavior. It could potentially enhance their quality of life and positively impact various negative consequences of addiction or factors involved in relapse, such as sleep, nutrition, self-esteem, impulsivity, craving, cognition, brain plasticity, and neuroinflammation.
However, physical activity programs conducted in AUD indicate a significant dropout rate, exceeding 40%. Supervising and individualizing the physical activity proposed to patients could reduce the dropout rate. We thus conducted a literature review that suggests adapting the physical activity of patients with severe Alcohol Use Disorder (AUD) by considering the triadic neurocognitive model of addiction. It is also essential to examine the specific barriers and facilitators to physical activity in patients with AUD.
We aim to investigate the effect of adapted physical activity introduced at the onset of detoxification during hospitalization for alcohol use disorder, as well as after discharge. Our focus is particularly on the impact on detoxification, sleep, impulsivity, craving, and cognitive functioning. We hypothesize that by improving these parameters, it may be possible to reduce the risk of relapse.
Our specific objectives are thus:
- To study the motivations and barriers to physical activity in patients suffering from AUD,
- To evaluate the feasibility, acceptability, and the ideal modalities of adapted physical activity offered to patients with AUD,
- To assess “in real life” the impact of adapted physical activity on the physical and mental health of patients, their cognitive functioning, and their addictive disorder during hospitalization and after discharge

Biomarkers in AUD
Leader: Laurent Coulbault
Nutritional status is often disturbed in patients with alcohol use disorder (AUD) and is related to the direct effects of alcohol but also to the metabolic burden of alcohol transformation and elimination. Nutritional disturbances involve deficits and perturbations of metabolism of many vitamins, such as thiamine (vitamin B1), nicotinamide (vitamin B3) or pyridoxine (vitamin B6). This facilitates the development of chronic diseases but also neurological and cognitive disorders, particularly in a context of alcohol withdrawal.
Although progress has been made in the management of patient care, clinicians still lack reliable biological markers of alcohol exposure and vitamin nutritional status, but also predictive biomarkers of severity of alcohol withdrawal. All these indicators could contribute to better patient care. Therefore, our main objectives are:
- 1) to better understand nutritional factors and pathophysiological mechanisms that may play a role in the development of severe cognitive disorders, such as Korsakoff syndrome, but also in the development of severe complications of alcohol withdrawal, such as delirium tremens,
- 2) to improve management of AUD patients by the transfer and the use of these innovative biological markers in a clinical setting.
This is currently being achieved by identifying and assessing biological markers in blood samples of AUD patients using mass spectrometry approaches. We are particularly interested in little-known thiamine metabolites that can interfere with cellular energy metabolism, but also by many tryptophan metabolites that can modulate glutamatergic pathways in the brain. Innovative markers of alcohol exposure (e.g. Phosphatidylethanol) are also evaluated to test their reliability and their impact in the management of these patients.
Sleep disorders
Leader : Alice Laniepce
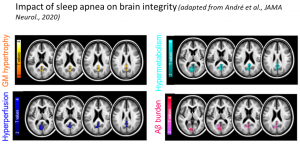
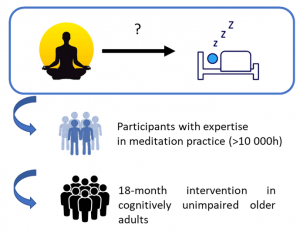
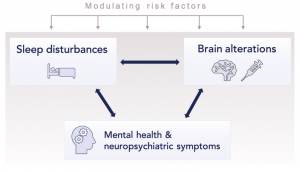
Sleep disturbances are frequent in patients with severe AUD and remain largely neglected even though they can persist after drinking cessation and are known to affect treatment outcome. Although studies have shown the contribution of sleep in cognitive functioning in healthy controls, the role of alcohol-induced sleep disturbances in the pathophysiology of alcohol-related brain and cognitive deficits remains unexplored.
The goals are :
- 1) to better understand alcohol-induced sleep alterations combining subjective (sleep diaries, questionnaires) and objective (polysomnography and actigraphy) methods,
- 2) to examine the relationship between sleep alterations, brain and cognitive alterations in patients with severe Alcohol Use Disorder (sAUD).

Cognitive and brain pathophysiology
Leader : Anne Lise Pitel (collaboration Shailendra Segobin, Inserm U1077)
The effects of AUD on brain and cognition are both direct via the neurotoxicity of ethanol and indirect through the impact of withdrawal, liver dysfunction, poor nutrition and sleep disorders. Both the structure and function of the brain can be affected when examined early in abstinence, with at least partial recovery with drinking cessation. Cognitive deficits and brain damage frequent at treatment entry can be considered as risk factors for relapse.
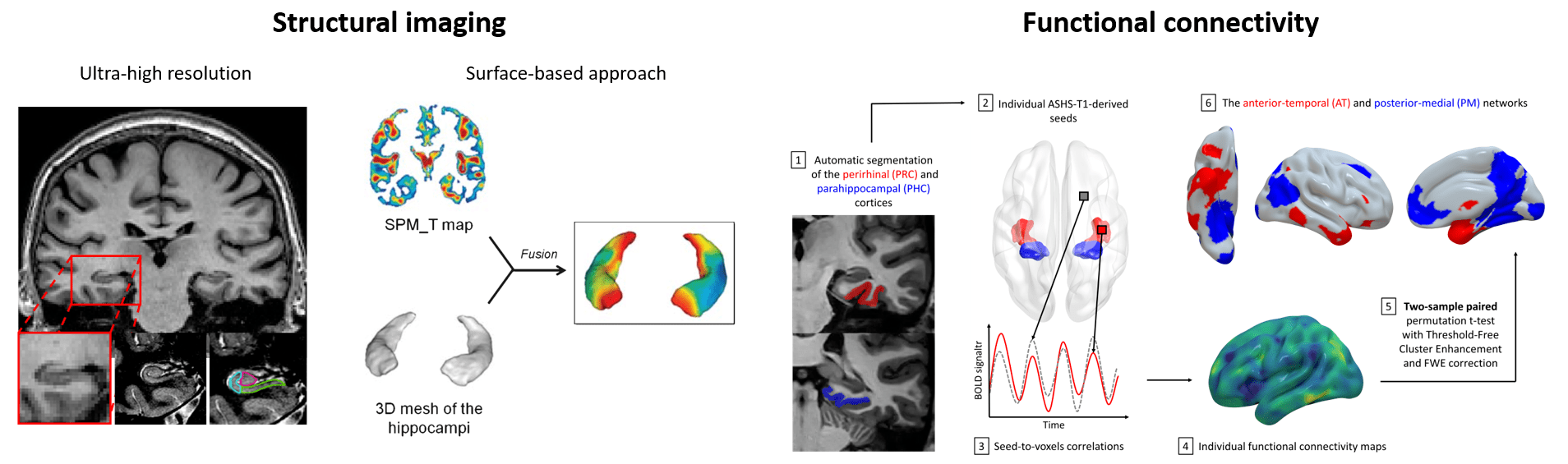
Our overall goal is to use standardized and specifically designed neuropsychological tasks, as well as structural (anatomical MRI and DTI) and functional (resting-state fMRI, ASL, PET) imaging techniques:
- 1. to unravel the temporal cascade of brain pathophysiological mechanisms leading to cognitive, emotional and behavioral impairments observed in AUD,
- 2. the direct and indirect impact of AUD on brain and cognition.
More precisely, we aim at:
- better describing certain cognitive or emotional processes in AUD,
- specifying structural and functional brain damage in AUD,
- investigating brain reorganization across key networks in AUD,
- better understanding of the heterogeneity of the cognitive deficits and brain damage observed in AUD,
- studying cognitive and brain changes with drinking cessation or relapse.

Korsakoff’s syndrome
Leader : Anne Lise Pitel (collaboration Shailendra Segobin, Inserm U1077)
Korsakoff’s syndrome (KS) is a permanent amnesic syndrome resulting from thiamine deficiency and developing most frequently in people with alcohol use disorder. People suffering from this condition have severe episodic memory problems, potentially accompanied by other cognitive, motor and neuropsychiatric disorders. In France, little is known about this condition, SK patients receive little consideration, are even stigmatized, and their care pathway from diagnosis to finding a suitable place to live is extremely chaotic. Developing new research programs on KS is therefore crucial. We are the only French research team and among the very few laboratories in the world to investigate KS, especially with neuroimaging techniques.
Our goal is twofold:
- 1 – To deepen our fundamental understanding of the pathophysiological mechanisms leading to this severe and debilitating condition.
- 2 – To improve the clinical prevention, diagnostic and care of KS patients, notably through the detection of AUD patients at risk to develop KS.
To this end, we compare patients with AUD with and without KS using psychological, neuropsychological, biological, sleep and neuroimaging (structural MRI, DTI, resting-state fMRI, FDG-PET) examinations.

Alcohol and aging
Leader : Anne Lise Pitel
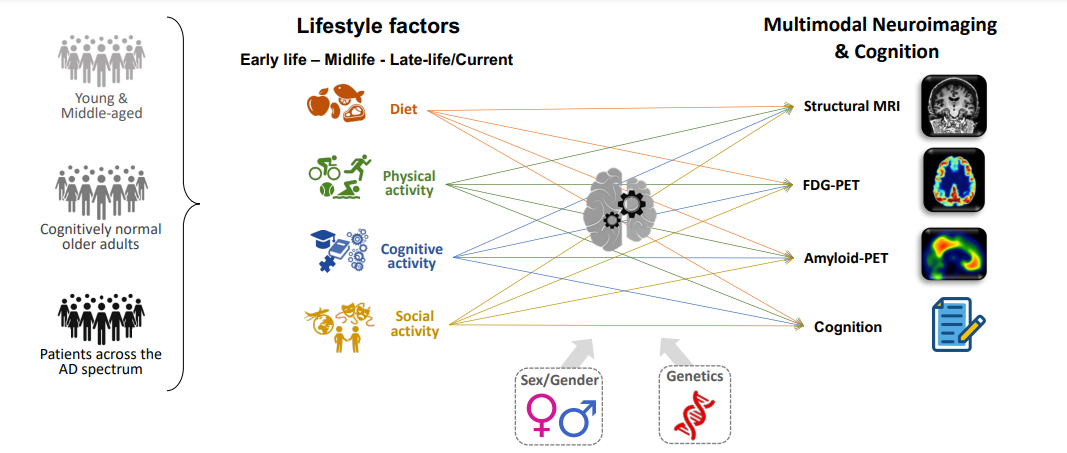
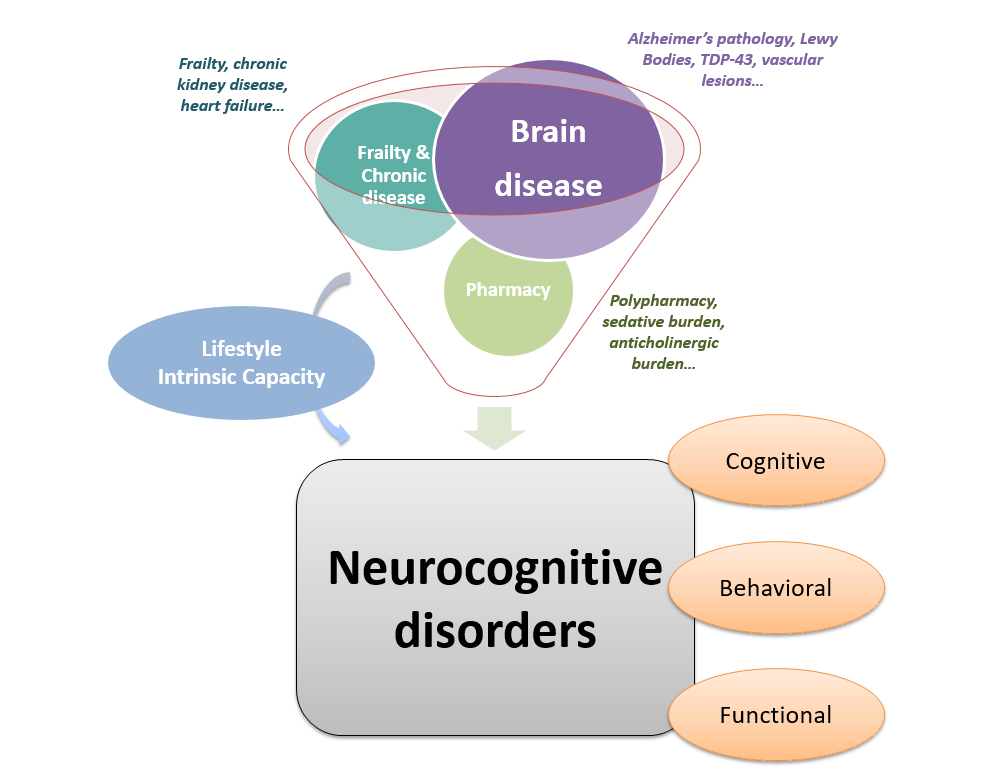
The effects of alcohol consumption are relatively well studied among young and middle-aged adults, but much less so among the elderly. And yet, in the elderly, alcohol consumption is associated with a high risk of falls, malnutrition, delirium and cognitive impairment. An interaction has been described between the effects of age and AUD: older patients with AUD have smaller volumes in certain brain regions than expected for their age, leading to the accelerated aging hypothesis.
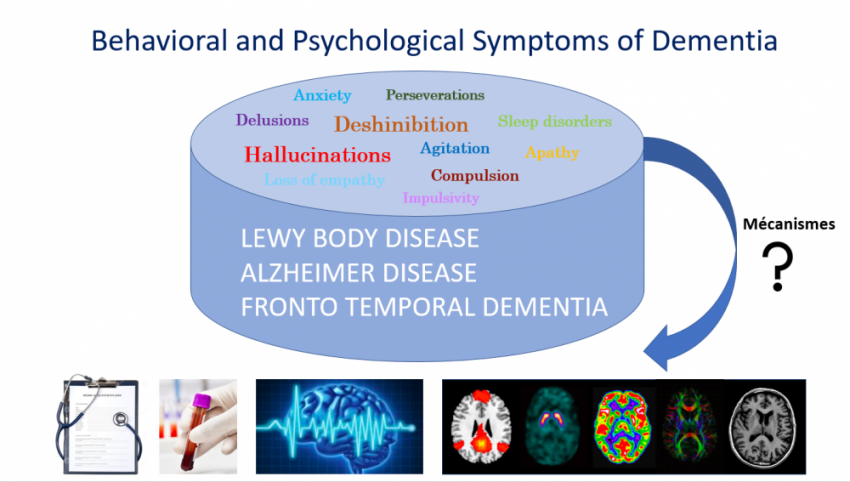
In addition, chronic and heavy alcohol consumption increases the risk of neurodegenerative diseases. However, the scientific evidence is mainly based on epidemiological or animal studies, and the mechanisms involved have not been fully explored. As a result, the impact of AUD on the development and/or progression of neurodegenerative diseases, particularly Alzheimer’s disease, remains very poorly understood.
Our goals are:
- to study, in older subjects, the effect of alcohol consumption through the lifetime on brain and cognition,
- to examine the cognitive and cerebral aging of older AUD patients,
- to compare neuropsychological performance and brain integrity in patients with neurocognitive disorders related to alcohol and Alzheimer disease taking into account the severity or stage of the clinical condition (AUD versus Mild Cognitive Impairment; Korsakoff’s syndrome versus Alzheimer dementia),
- to investigate brain and blood biomarkers of Alzheimer disease in patients with AUD and Korsakoff’s syndrome.
Our laboratory has unique sets of multimodal data collected in patients with AUD, Korsakoff’s syndrome, Mild Cognitive Impairment and Alzheimer disease, which enable us to conduct very original retrospective analyses. We also conduct prospective studies of these patient groups with a design including novel blood and PET biomarkers of Alzheimer disease.