Neurodegenerative diseases
Principal Investigators: Sophie Dautricourt, Géraldine Poisnel, Julie Gonneaud, Gaël Chételat, Robin de Flores, Antoine Garnier-Crussard
The axis of Neurodegenerative diseases addresses 7 themes:
- Behavioral and Psychological Symptoms of Dementia PI: Sophie Dautricourt
- Blood-based biomarkers in ageing and dementia PI: Géraldine Poisnel
- Lifestyle factors in ageing and Alzheimer's disease PI: Julie Gonneaud
- Meditation and lifestyle-based intervention to promote healthy ageing and prevent dementia PI: Gaël Chételat
- Multimodal imaging of the medial temporal lobe PI: Robin de Flores
- Multimodal neuroimaging and computational modeling in ageing and Alzheimer’s disease PI: Gaël Chételat
- Systemic disorders & brain lesions interactions PI: Antoine Garnier-Crussard
Behavioral and Psychological Symptoms of Dementia
Leader: Sophie Dautricourt
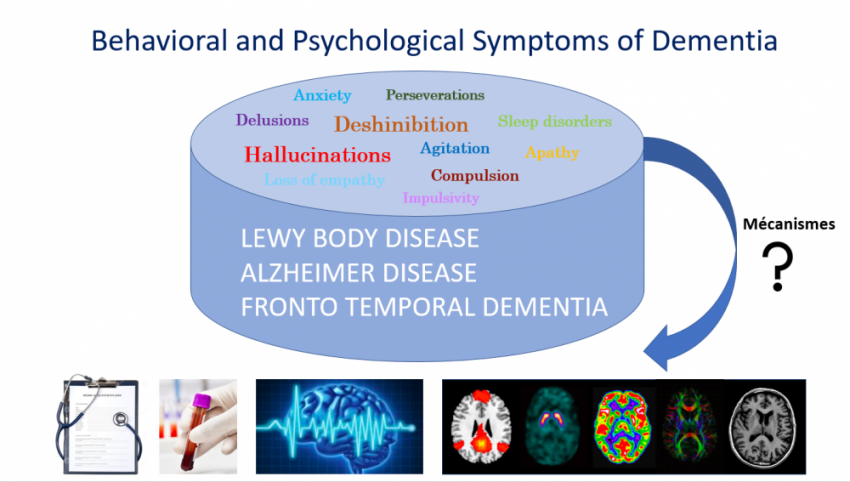
Behavioral and Psychological Symptoms of Dementia (BPSD), also called neuropsychiatric symptoms (NPS) are highly common in the course of neurodegenerative diseases. They include a wide range of symptoms, such as agitation, aggression, impulsivity, delusions, hallucinations, depression, anxiety, apathy, deshinibition, loss of empathy, perseverations, compulsions, sleep and appetite disorders.
BPSD affect various neurodegenerative disease, such as Alzheimer’s disease, Lewy body demantia, fronto-temporal dementia, and vascular dementia. They are associated with worst cognitive and functional prognosis, and with higher patient and caregiver distress.
The Behavioral and Psychological Symptoms of Dementia research topic aims at understanding the brain mechanisms underlying Behavioral and Psychological Symptoms of neurodegenerative diseases.
To this aim, we use multimodal neuroimaging, blood and cerebrospinal fluid biomarkers in combinaison with clinical, cognitive, sleep and behavioral assessments, to investigate the pathophysiological mechanisms underlying BPSD.
Blood-based biomarkers in ageing and dementia
Leader: Géraldine Poisnel
There is an increasing emphasis on development and use of blood-based biomarkers :
- For diagnosis and prediction of dementia,
- To identify underlying pathophysiological mechanisms
- To serve as intermediate outcome measures to monitor response to interventions.
We aim to understand how blood-based biomarkers—such as those linked to chronic stress, telomeres, inflammation, and early Alzheimer’s disease (AD) processes—contribute to physiological and pathological ageing, neurodegeneration, and dementia risk. We also investigate how lifestyle and psychoaffective factors, including interventions like long-term meditation, influence these biological processes and shape brain and cognitive aging.
To support our research, we use the IMAP+ and Age-Well trials, which provide comprehensive data on blood-based biomarkers, cognition, lifestyle, and brain imaging. These resources enable integrative multimodal analyses to clarify the role of biomarkers in aging and dementia and to develop composite measures like allostatic load (AL), reflecting the cumulative impact of chronic stress. We also explore brain-derived extracellular vesicles (EVs) from plasma as innovative biomarkers of brain changes.
Our ultimate goal is to uncover mechanisms of brain ageing and support personalized, non-invasive prevention strategies for dementia.

Lifestyle factors in ageing and Alzheimer's disease
Leader: Julie Gonneaud
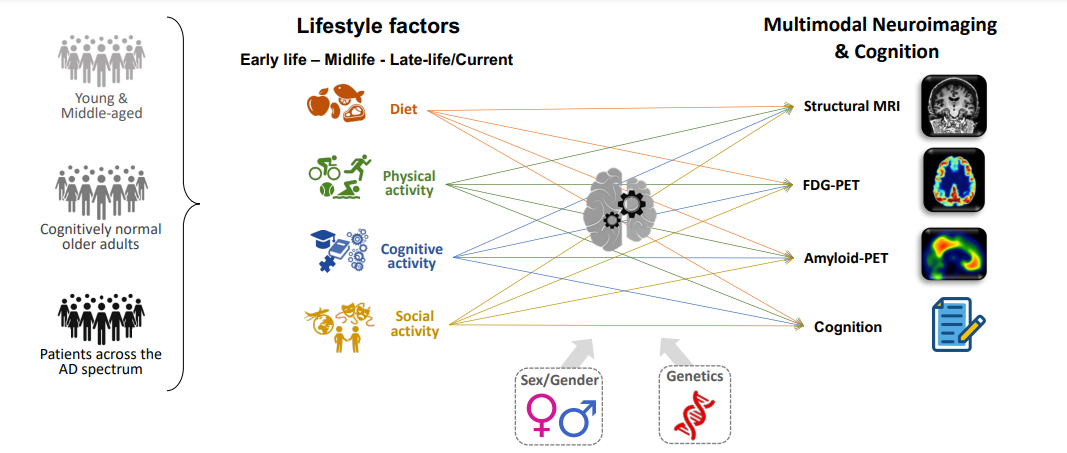
There is growing evidence in the literature that we could modify the course of neurodegenerative diseases, and brain and mental health in general, by modifying our lifestyle. A recent review suggests that ~45% of dementia cases could be prevented by acting on modifiable risk factors, including lifestyle factors (Livingston et al., Lancet, 2024). The Lifestyle factors in ageing and Alzheimer’s disease research topic focuses on understanding the brain mechanisms underlying lifestyle influences, spanning from normal aging to Alzheimer’s disease dementia, and examining how sex/gender and genetics could modulate these associations.
To achieve this, we use cognitive assessments and multimodal neuroimaging—such as structural MRI, functional MRI, FDG, and amyloid-PET—in combination with lifestyle evaluations (e.g., education level,
cognitive, physical, and social engagement, and diet).
We are particularly interested in (i) understanding the brain mechanisms of reserve across the lifespan, (ii) assessing the combined and relative effects of lifestyle factors on cognitive and neuroimaging outcomes (iii) identifying critical periods during which lifestyle factors may have the greatest impact.
In this research topic, we place particular emphasis on deepening our understanding of the roles of sex/gender and genetics in aging and dementia, especially in how they may modulate the relationship between
lifestyle factors and cognitive/brain health outcomes.
Meditation and lifestyle-based intervention to promote healthy ageing and prevent dementia
Leader: Gaël Chételat
We aim at better identifying the factors that could promote healthy ageing and prevent or delay Alzheimer’s disease and dementia in general. Notably, we are coordinating a large European project (www.medit-ageing.eu) assessing the effects of meditation training both in a population of expert meditators and in cognitively unimpaired elderly who were proposed an original 18-month meditation program. Multiple complementary neuroimaging techniques are used to assess the impact on brain health but also the underlying mechanisms.

Multimodal imaging of the medial temporal lobe
Leader: Robin de Flores
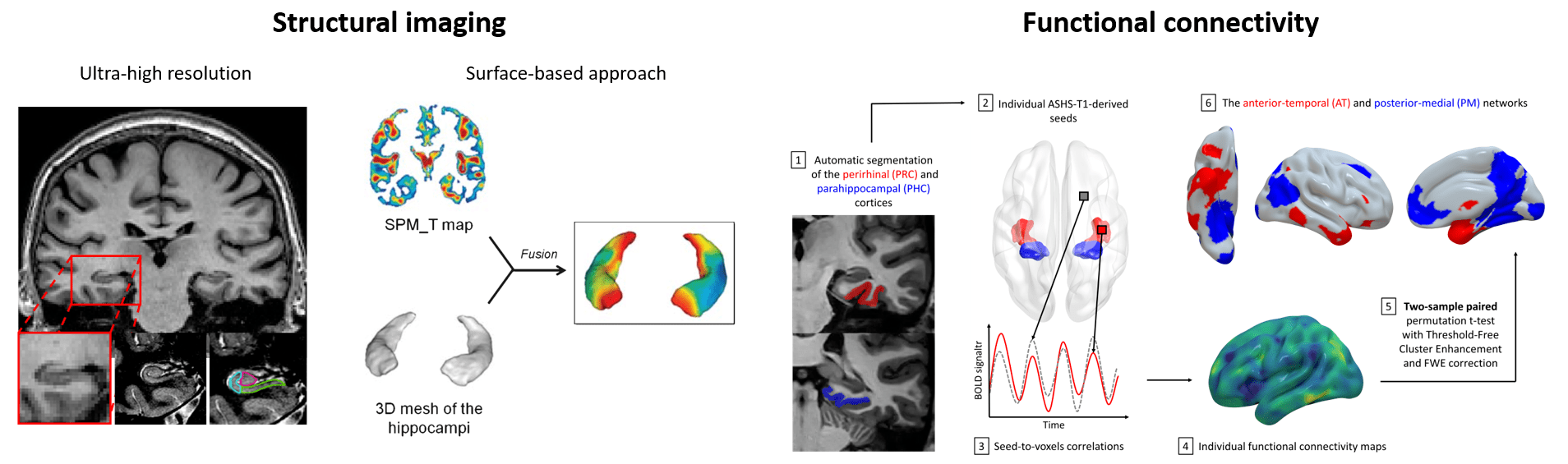
The medial temporal lobe (MTL) is one of the most studied brain regions because of its involvement in a myriad of cognitive processes and its sensitivity to ageing, neurological and psychiatric diseases. Importantly, MTL subregions – including hippocampal subfields – are differentially i) affected in different conditions (eg normal ageing vs Alzheimer’s disease) and ii) involved in cognitive functions. Thus, we aim at providing a granular description of the alterations and functioning of the MTL and its subregions using advanced multimodal imaging techniques. More precisely, we investigate two specific topics:
Structural imaging : In 2010, we developed an ultra-high resolution MRI sequence together with a manual segmentation protocol to precisely estimate hippocampal subfields volumes. We then improved our sequence and now use Automatic Segmentation of Hippocampal Subfields (ASHS). In addition, we use a surface-based approach based on voxelwise analyses coupled with 3D hippocampal surface mapping. These techniques were applied to evaluate the pattern of atrophy in diverse populations, including in patients across the Alzheimer’s disease continuum. Our group is also contributing to the Hippocampal Subfields Group (www.hippocampalsubfields.com), an international collaborative project aiming at standardizing hippocampal subfields delineation.
Functional connectivity : Since the MTL is highly connected to the rest of the brain through specific networks, we use resting-state fMRI data with a seed-based correlation approach to study i) hippocampal subfield networks and ii) the anterior temporal and posterior medial systems.
Multimodal neuroimaging and computational modeling in ageing and Alzheimer’s disease
Leader: Gaël Chételat
We use multimodal neuroimaging techniques and computational modelling to investigate the pathophysiological mechanisms of Alzheimer’s disease and identify early biomarkers of cognitive decline. The populations we are interested in range from cognitively normal individuals (young to elderly adults to investigate normal ageing processes) to patients with subjective cognitive decline, mild cognitive impairment and dementia. We are also especially interested in the psycho-affective risk-factors (depression, stress, anxiety), their links with brain integrity and how they could be prevented.
Systemic disorders & brain lesions interactions
Leader: Antoine Garnier-Crussard
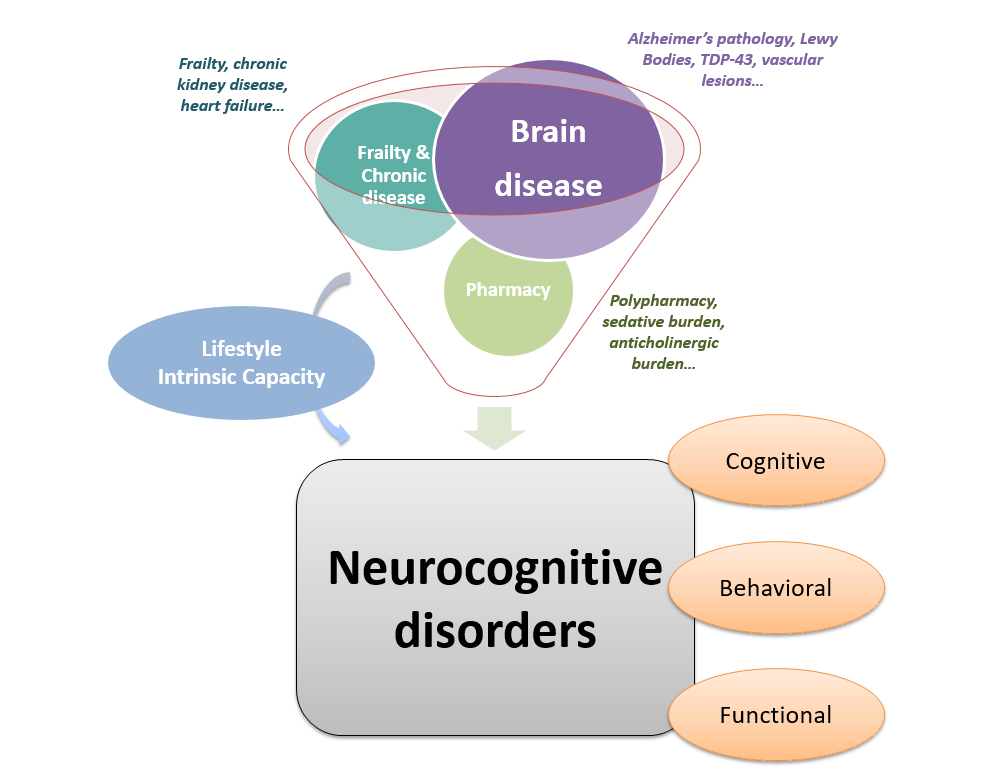
This research topic focuses on an holistic approach of neurocognitive disorders, aiming at disentangle multiple factors leading to cognitive, behavioral and functional changes in patient with neurocognitive disorders. Indeed, brain diseases (such as Alzheimer’s pathology) lead to neurodegeneration and cognitive symptoms, but several other factors “beyond the brain” also contribute to symptoms and can influence the clinical phenotype as well as the complications of the disease. We specifically focus on frailty, chronic disease and polypharmacy in addition to brain lesions (measured in vivo with biomarkers) to better explain at the individual levels the predictors of clinical changes.
For example, we study in older adults with neurocognitive disorders the respective impact of brain lesions (notably white matter hyperintensities measured with structural MRI, Alzheimer’s biomarkers measured with PET-scan, CSF or plasma), frailty (measured with Fried phenotype or frailty index), intrinsic capacities (measured with WHO-based tools) and medication (notably anticholinergic burden measured with the Drug Burden Index) and their relationships, to better understand and predict cognitive decline, behavioral symptoms and loss of autonomy.
At the era of disease-modifying therapies in Alzheimer’s disease, a better understanding of the origin of each symptom, at each stage, for each patient is critical.