Sleep disorders
Principal Investigators: Géraldine Rauchs, Claire André, Alice Laniepce
The axis of Sleep disorders addresses 6 themes:
- Sleep, imaging and memory consolidation PI: Géraldine Rauchs
- Sleep, brain integrity and cognition PI: Géraldine Rauchs
- Sleep apnea, brain alterations and modulation by lifestyle factors PI: Géraldine Rauchs
- Sleep and meditation practice PI: Géraldine Rauchs
- Sleep disturbances, mental health and neuropsychiatric symptoms PI: Claire André
- Sleep disorders PI: Alice Laniepce
Sleep, imaging and memory consolidation
Leader: Géraldine Rauchs
Sleep is a physiological state that promotes memory consolidation. In the team, we aim at characterizing the impact of age-related changes in sleep architecture and micro-structure on sleep-dependent memory consolidation. We have recently shown that the temporal dynamics of sleep spindles is altered during aging. The proportion of fast spindles organized in temporal clusters decreased non-linearly with age and the mean size of spindle clusters was positively associated with memory consolidation and negatively with NREM sleep micro-arousal density. These results suggest that clusters of fast spindles may constitute stable sleep periods promoting off-line processes such as memory consolidation. We are further investigating sleep-dependent memory consolidation in older adults by analyzing resting-state functional connectivity data. This work is carried out in collaboration with Dr Alison Mary (Brussels, Belgium).

Sleep, brain integrity and cognition
Leader: Géraldine Rauchs
We are one of the few teams in the world to have particularly rich sleep data, including questionnaires, actigraphy, polysomnography, and data from a wearable device, to reflect the full complexity of sleep, combined with multimodal imaging data (structural MRI, DTI, resting-state fMRI, FDG-PET, amyloid-PET, high-resolution MRI of the hippocampus). We study in depth the associations between sleep and cognitive and brain alterations. We are particularly interested by new wearable devices that allow us to assess variability in sleep quality from one night to the next and its impact on amyloid accumulation, and more generally on brain integrity.

Sleep apnea, brain alterations and modulation by lifestyle factors
Leader: Géraldine Rauchs
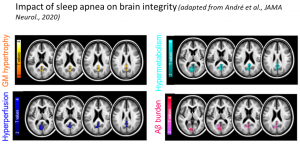
We are characterizing the impact of sleep apnea on brain alterations. We published a first study showing that sleep apnea is associated with increases in grey matter volume, brain perfusion and metabolism, and greater amyloid deposition in the posterior cingulate cortex and the precuneus (André et al., JAMA Neurology, 2020). We are pursuing this work by focusing on white matter integrity, exploring gender differences as well. Finally, we are also investigating whether cognitive reserve and physical activity can modulate the impact of apneas on cognitive and brain alterations. This last part of our project is carried out in collaboration with Dr Julie Gonneaud, also a member of the Neuropresage team!
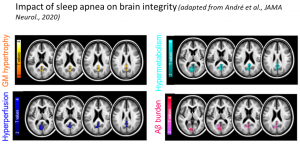
Sleep apnea, brain alterations and modulation by lifestyle factors
Leader: Géraldine Rauchs
We are characterizing the impact of sleep apnea on brain alterations. We published a first study showing that sleep apnea is associated with increases in grey matter volume, brain perfusion and metabolism, and greater amyloid deposition in the posterior cingulate cortex and the precuneus (André et al., JAMA Neurology, 2020). We are pursuing this work by focusing on white matter integrity, exploring gender differences as well. Finally, we are also investigating whether cognitive reserve and physical activity can modulate the impact of apneas on cognitive and brain alterations. This last part of our project is carried out in collaboration with Dr Julie Gonneaud, also a member of the Neuropresage team!
Sleep and meditation practice
Leader: Géraldine Rauchs
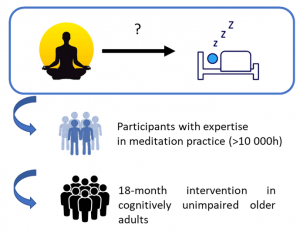
As sleep disturbances are increasingly recognized as a potential risk factor of cognitive decline and Alzheimer’s disease, it is crucial to improve the management of sleep disorders in older populations, and especially in at-risk individuals of dementia, in order to promote successful aging.
To this end, we are currently investigating the effect of meditation practice on sleep quality as assessed with the different tools mentioned above. We have conducted two studies: the first one in participants experts in meditation practice compared to meditation-naïve individuals, and the second is an 18-month intervention study in cognitively unimpaired older adults.
Sleep disturbances, mental health and neuropsychiatric symptoms
Leader: Claire André
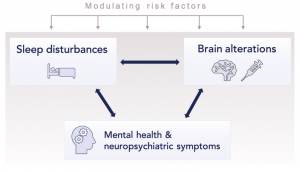
Sleep disturbances are frequent in older populations, and even more common and severe in neurodegenerative diseases. They have been associated with a wide range of negative cerebral and cognitive outcomes, and greater dementia risk. As sleep plays a crucial role in emotions regulation, we work on clarifying whether age-related sleep disturbances could also be associated with mental health issues in aging, and the emergence of neuropsychiatric symptoms in neurodegenerative diseases. We combine multimodal neuroimaging, blood biomarkers, neuropsychological and behavioral measures, and detailed sleep examinations (questionnaires, sleep diaries, actigraphy and polysomnography data) to address the following goals:
- Unravel which aspects of sleep are associated with anxiety, depression, ruminations and worry in older populations and patients with neurodegenerative diseases. We have a particular interest for the role of REM sleep disturbances, sleep fragmentation, sleep debt and obstructive sleep apnea.
- Investigate underlying brain mechanisms and the impact of neurodegenerative processes (e.g., amyloid and tau pathologies) on these associations.
- Determine which factors modulate these links (e.g., sex, genetic risk factors, lifestyle), to identify particularly vulnerable groups of individuals.
We use multi-cohort data in the context of an international collaboration to reach large sample sizes to tackle these questions.
Sleep disorders
Leader: Alice Laniepce
Sleep disturbances are frequent in patients with severe AUD and remain largely neglected even though they can persist after drinking cessation and are known to affect treatment outcome. Although studies have shown the contribution of sleep in cognitive functioning in healthy controls, the role of alcohol-induced sleep disturbances in the pathophysiology of alcohol-related brain and cognitive deficits remains unexplored.
The goals are :
- 1) to better understand alcohol-induced sleep alterations combining subjective (sleep diaries, questionnaires) and objective (polysomnography and actigraphy) methods,
- 2) to examine the relationship between sleep alterations, brain and cognitive alterations in patients with severe Alcohol Use Disorder (sAUD).
